Maximize efficiency & profitability by delivering a consistent customer experience across sales channels. Connect your enterprise apps with DCKAP Integrator - the No. 1 ERP integration platform for distributors.
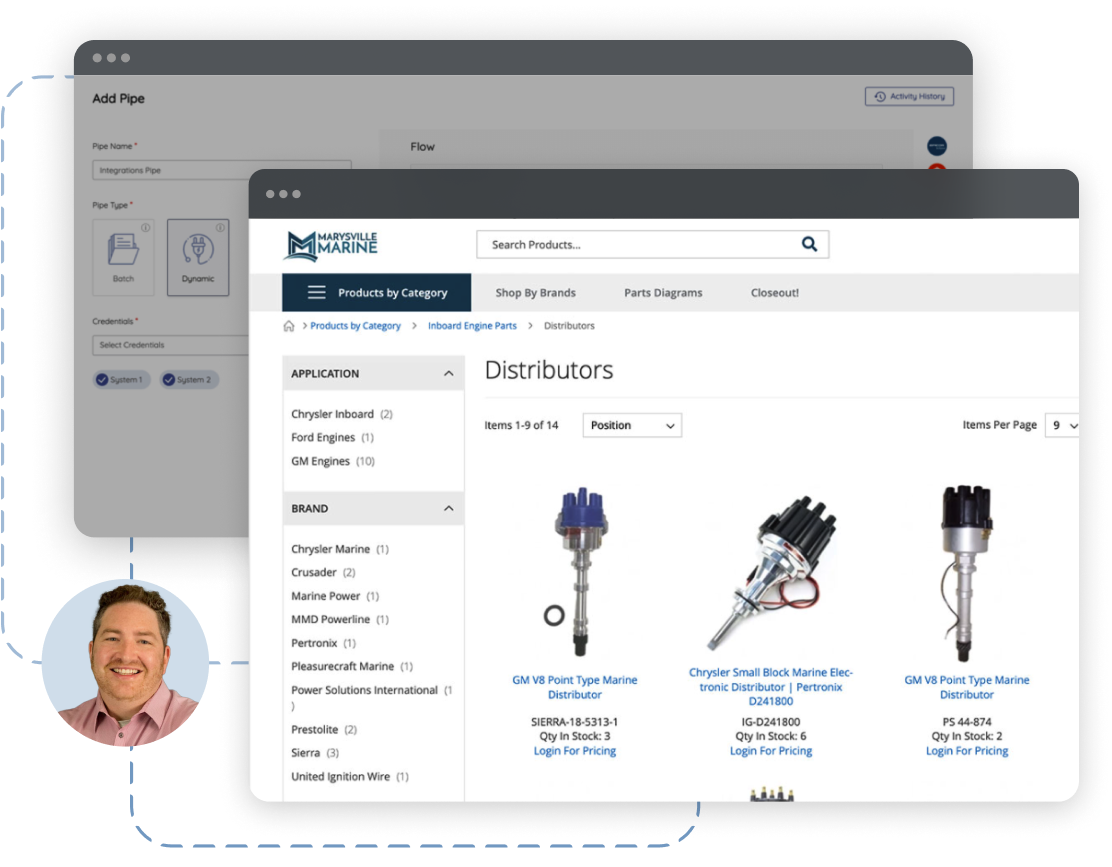
Stop jumping back and forth between systems. Connect, automate, and sync data between your CRM, ecommerce platforms, and popular ERPs such as Oracle Netsuite, Epicor Prophet 21, DDI Inform, Infor, Distribution One, Microsoft Dynamics 365, Sage & many more.
When you have multiple ecommerce sites and tens of thousands of SKUs across hundreds of storefronts and distribution centers, things can get complicated. Our intuitive platform simplifies ecommerce.
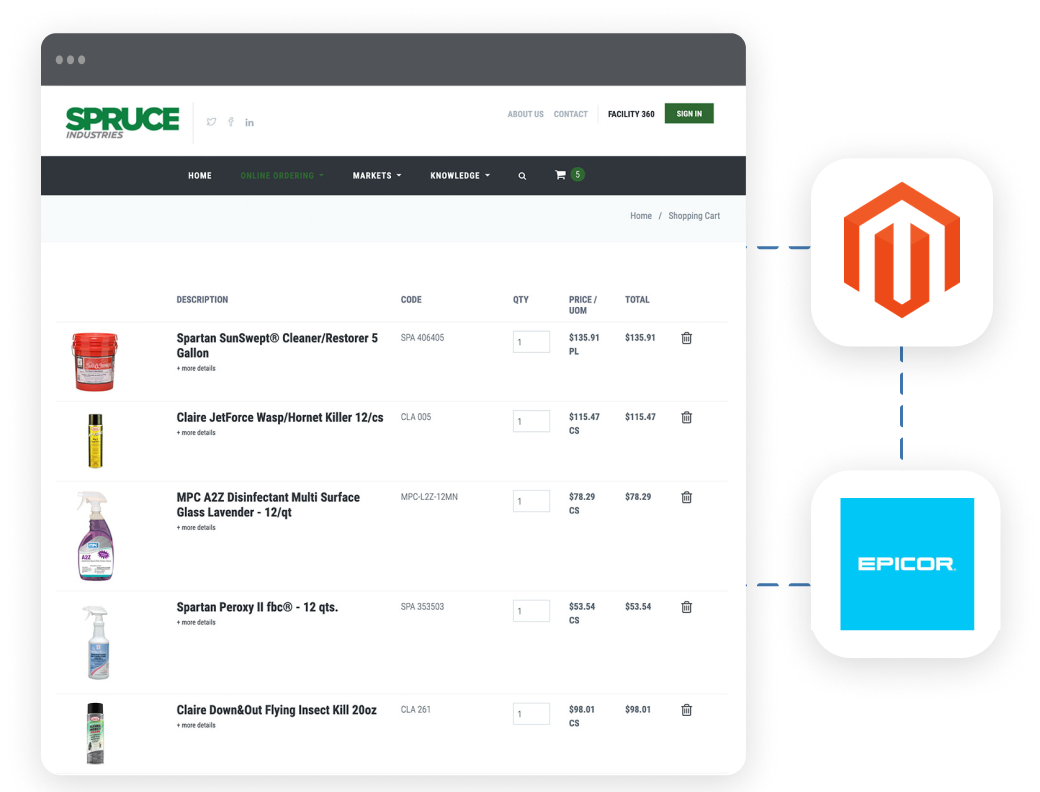
Automate workflow, maintain data integrity, reduce errors and more with DCKAP Integrator. Your organization will run at peak efficiency making it easier for your busy customers to shop and buy.
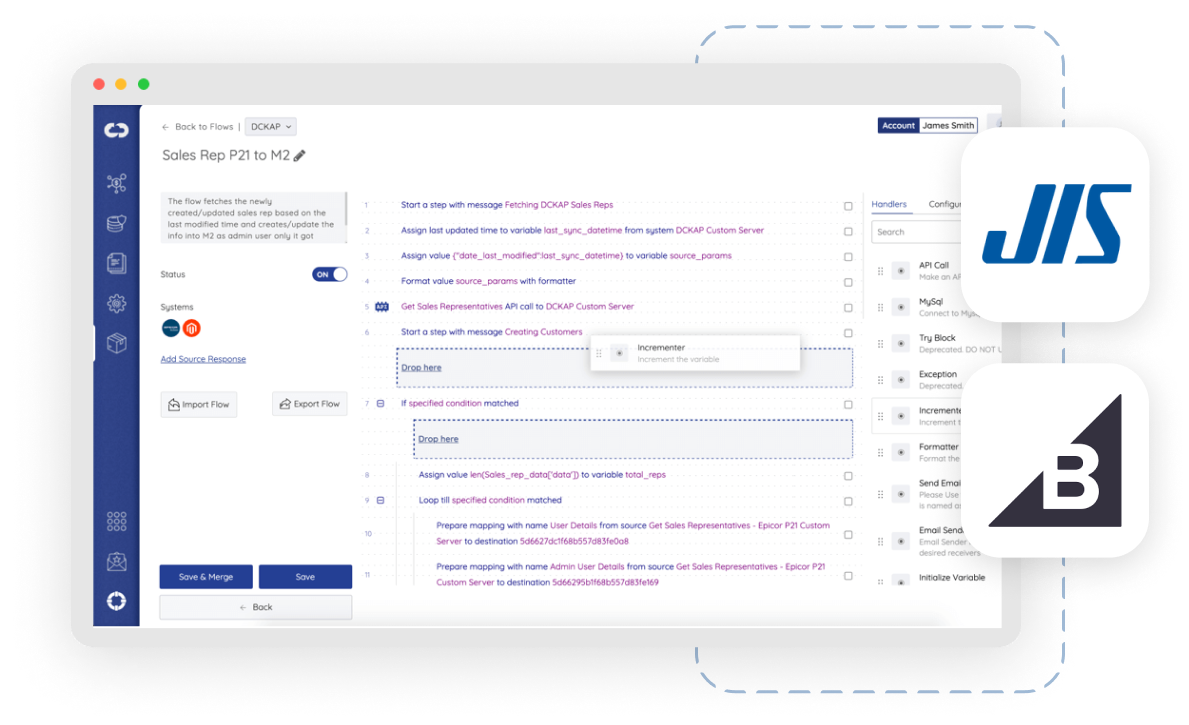
Built-in templates, drag-and-drop functionality and the intuitive DCKAP Integrator dashboard make getting new solutions online – and connected with other essential systems – seamless.